Vaccine Prioritization for Type 1 diabetics and diabetics other than Type 2 in the U.S.
Like all things COVID in the U.S., this is a mess already.
In November, I tweeted some thoughts on where people with diabetes may fall in the COVID-19 vaccine prioritization in the United States. I had been haunted by this list of people who may be at increased risk of severe illness due to “Certain Medical Conditions” that the CDC has been maintaining on their website.
I wasn’t proud of myself for tweeting out this thread at the time—it was pure speculation. The item of interest is how the CDC splits people with diabetes into “are at increased risk” (Type 2) and “might be at an increased risk” (Type 1).


Now that we have vaccines and are vaccinating health care personnel and long term care facility residents (Phase 1a), states are beginning to think of vaccine prioritization for the next phases. Ultimately, these decisions are state, or even county-based, but the Advisory Committee on Immunization Practices (ACIP) under the CDC is also putting out guidance on who should be prioritized next. The current ACIP recommendation for allocation outlines guidance for Phases 1b and 1c.
To summarize, Phase 1b includes essential workers and persons aged 75 and over. Phase 1c includes “persons aged 65–74 years, persons aged 16–64 years with medical conditions that increase the risk for severe COVID-19, and essential workers not previously included in Phase 1a or 1b.” Without any other prioritization status, people with diabetes should be falling under Phase 1c.
However, this is where that “are at increased risk” (Type 2) and “might be at an increased risk” (Type 1) distinction matters. The footnote for the “medical conditions that increase the risk for severe COVID 19” in the ACIP recommendation is the following:
Adults of any age with the following conditions are at increased risk for severe COVID-19–associated illness: cancer; chronic kidney disease; chronic obstructive pulmonary disease (COPD); heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies; immunocompromised state (weakened immune system) from solid organ transplant; obesity (body mass index [BMI] ≥30 kg/m2 but <40 kg/m2); severe obesity (BMI ≥40 kg/m2); sickle cell disease; smoking; type 2 diabetes mellitus; and pregnancy. No data are currently available on the safety of COVID-19 vaccines in pregnant persons. If pregnant persons are part of a group that is recommended to receive a COVID-19 vaccine (e.g., health care personnel or essential worker), they may choose to be vaccinated. A conversation between the patient and the patient’s clinical team might assist with decisions regarding the use of vaccines approved under EUA for the prevention of COVID-19. Guidance for pregnant persons will be updated as new data becomes available at https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html. The list of high-risk medical conditions is updated routinely as new data becomes available at https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
The ACIP recommendation does not include people with type 1 diabetes (or any other type of diabetes than type 2) in their recommendation for Phase 1c. After Phase 1c, all that is left is Phase 2, which includes everyone else.
Why should the CDC prioritize people with all types of diabetes?
Well, several high-quality studies indicate that people with type 1 diabetes are at just as much, if not more, risk than people with type 2 diabetes. Thank you to James Elliott and the folks on his thread who unearthed and summarized these. The “OR” indicates odds ratios of hospitalization and severe illness — an odds ratio greater than 1 indicates that an event is “more likely to occur.” These studies indicate the risk for people with type 1 diabetes is double, if not triple, the risk that occurs in the general population.
1. Gregory et al., prospective cohort study in the US, whole Vanderbilt network, outcome: COVID-19 hospitalization
T1D OR 3.90 (95% CI 1.75-8.69)
T2D OR 3.36 (95% CI 2.49-4.55)
2. Barron et al., prospective cohort study in the UK, whole population of England, outcome: in-hospital COVID-19 death
T1D OR 3.51 (95% CI 3.16-3.90)
T2D OR 2.03 (95% CI 1.97-2.09)
3. McGurnaghan et al., prospective cohort study in the UK, whole population of Scotland, outcome: COVID-19 death or critical care
T1D OR 2.396 (95% CI 1.815-3.163)
T2D OR 1.369 (95% CI 1.276-1.468)
Insulin-dependent diabetics also need insulin or they die, often within days.
When insulin is still priced at $275 a vial and our health insurance system is largely employer-based, people with diabetes who aren’t “essential workers” but need to be on premise at work, have no choice but to show up. It’s a choice of risking death by COVID-19 or losing health insurance, not being able to afford insulin, and dying from insulin rationing. We will never forget Robert Washington, a 68-year old security guard, who returned to work because he needed the health benefits and paycheck to pay for insulin. He died of COVID-19 after returning to work.
Having type 1 diabetes alone could mean we are not prioritized for care in the event of overburdened hospitals and ICUs. On a good day, many people with type 1 diabetes have experienced providers managing bloodsugars in the hospital setting. During COVID-19 times, it feels certain that people with type 1 diabetes would not receive adequate treatment.
As people with type 1 diabetes, we do not have to be prioritized over people with type 2 diabetes. Personally, I believe that people with all types of diabetes should be prioritized in phase 1c together. It’s especially important to note people with diabetes other than type 1 and type 2—LADA, MODY, gestational, type 3c, steroid-induced, CFRD, etc. There has always been more than two types of diabetes, and when we focus on only type 1 and type 2, we risk not including others in the prioritization.
While expectations are certainly rosy (full population vaccination by spring or summer), this may not be the reality. It could mean a delay of weeks or months for some people with diabetes. This is not acceptable.
Who is urging the CDC to prioritize all people with diabetes?
On December 4th, 2020, the Vanderbilt researchers from that study urged prioritization for people with type 1 diabetes.
On January 11, 2021, individuals and grassroots diabetes organizations, including T1International and many of their state chapters, signed onto a letter to CDC and ACIP members urging prioritization for people with type 1 diabetes.

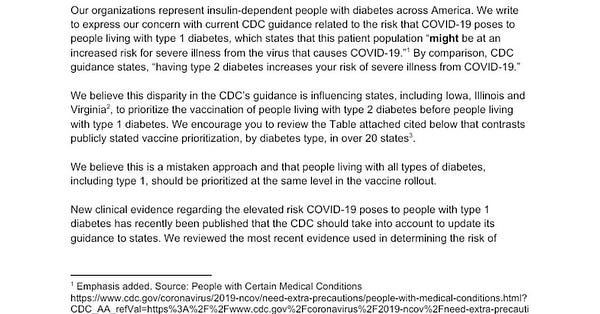
On January 13th, 2021, The American Diabetes Association and 18 other diabetes patient advocacy organizations sent a letter to the CDC urging them to update their guidance in regards to type 1 diabetes. Their COVID-19 hub claims to have distribution information on a state by state basis but simply links to the state vaccine websites only.
On January 18th, 2021, The Lancet also made the case for prioritization of people with type 1 diabetes.
What are the states actually doing?
Ultimately, vaccine prioritization and distribution are decisions being made at the state-level and county-level. As states prepare their plans for distribution phases, we are finding that many intend to follow the ACIP recommendations. As such, many states will also follow ACIP when making their recommendations and counties will likely follow the state recommendations.
So, the recommendations being made by ACIP that do not include people with diabetes other than type 2 are going to have ramifications for people with diabetes across the country.
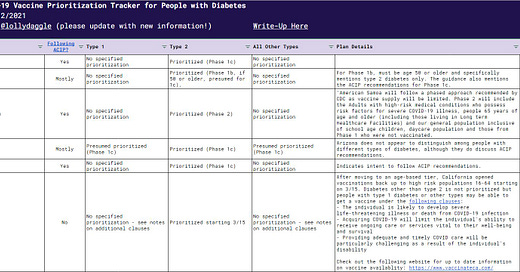
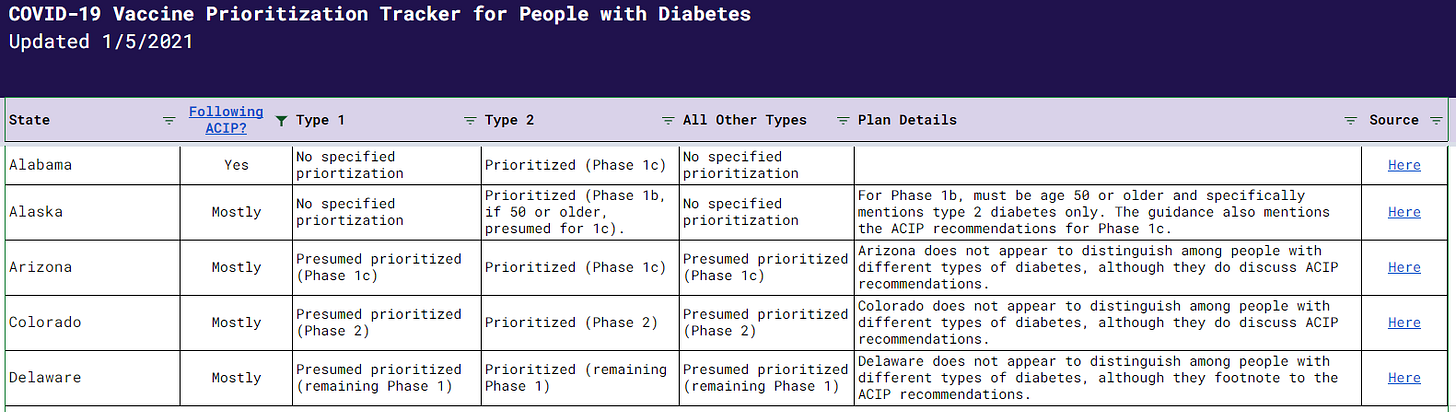
On Twitter, I put out a call to crowdsource what states are planning. I appreciate everyone in the community who chimed in! Special shoutout to Emily Piscreta and @official_allis for pitching in on several states.


The results of this thread are compiled in a state by state database. Use this information at your own risk! These timelines and distribution plans could possibly change as we are still in Phase 1a.
To summarize, here are some of the state by state findings:
A lot of states are following the ACIP recommendations to the tee, or indicate that they will. This means no prioritization right now for people with diabetes (other than type 2). These include, but are not limited to, Alabama, Arkansas, Connecticut, Georgia, Idaho, Illinois, Iowa, Kentucky, Louisiana, Maine, Minnesota, Mississippi, Montana, Nebraska, New Mexico, South Carolina, Vermont, Virginia, and Wisconsin.
In other states, it is clear they are using the ACIP recommendations as a framework but may be adjusting slightly. For instance, some states do not distinguish between people with different types of diabetes. Other states simply link to the “Certain Medical Conditions” page that does distinguish between type 1 and type 2 for their definition of those who are at high risk. In these states, it is unclear if people with type 1 (or other types) would ultimately be prioritized.
Ohio is prioritizing people with type 1 diabetes as part of their Phase 1B but does not indicate prioritization for people with any other type of diabetes. This is a very different approach compared to how other states are mirroring ACIP.
Most states and counties are likely to work off of an honor system. Washington State outlines details of their honor system tool here. In other states, when you reach the portal/ registration level (whether at the state or county level), it may not distinguish between types of diabetes or ask about high risk conditions in general. There may be room to squeeze in during a prioritization phase.
After going through these states, a lot of the guidance isn’t clear or specific yet! Hopefully, clarity comes as we move into the next phases. This is an opportunity for states to make life easier for everyone by including people with all types of diabetes in a priority group.
What action can we take to ensure people with all types of diabetes are being prioritized?
Several small diabetes organizations and individual patient advocates are drafting a letter to the CDC asking ACIP to consider these studies in their vaccine prioritization recommendations.
Contact all of your representatives. Your federal reps may be able to place pressure on the CDC. Your state and county reps may have influence over the local prioritization plans. Also, contact your state and county departments of health.
Help us keep this state by state database updated as more information becomes available! I’ve turned edit access on here.
If you are in Virginia, please get in contact with me!
You can reach me on Twitter or at hannah.m.crabtree@gmail.com with any recommendations or updates.